Pediatric cancer research funding is less than 4%.
Our Gifts of Hope help fund pediatric brain cancer research projects. Through medical advisors we dedicate funds that show promise of medical advancement, clinical trials, and new treatments. With your support, we can change the prognosis of rare and difficult to treat brain tumors such as DIPG and ATRT.
With your support, we can create hope!
2021 – 2022 Gifts of Hope
For the last couple of years, Nelina’s Hope has been supporting Dr. Rutka’s preclinical trial research studies for a specialized procedure called High Intensity Focused Ultrasound (HIFU) at the Brain Tumor Research Centre at SickKids Hospital in Toronto. This procedure, developed by Sunnybrook Health Sciences Centre scientists, allows temporary disruption of the blood brain barrier to allow for more effective treatment directly at the site of the tumor.
We have learned that the preclinical trial research has concluded and a clinical trial for DIPG is before Health Canada for approval with initial rounds of patient enrollment beginning in early 2022. The trial will initially be looking at safety and feasibility in patients using established chemotherapies that don’t cross the blood brain barrier on their own.
In looking ahead to later phases of the clinical trial, experiments are now being conducted to find drug candidates and/or combinations of drugs that could be used in later stages of this trial that would test efficacy of treatment known to target Diffuse Midline Glioma/Diffuse Intrinsic Pontine Glioma (DMG/DIPG) specifically based on genetic profiles of the tumor. We are excited to share that our 2021 – 2022 Gift of Hope will help support these initial experiments.
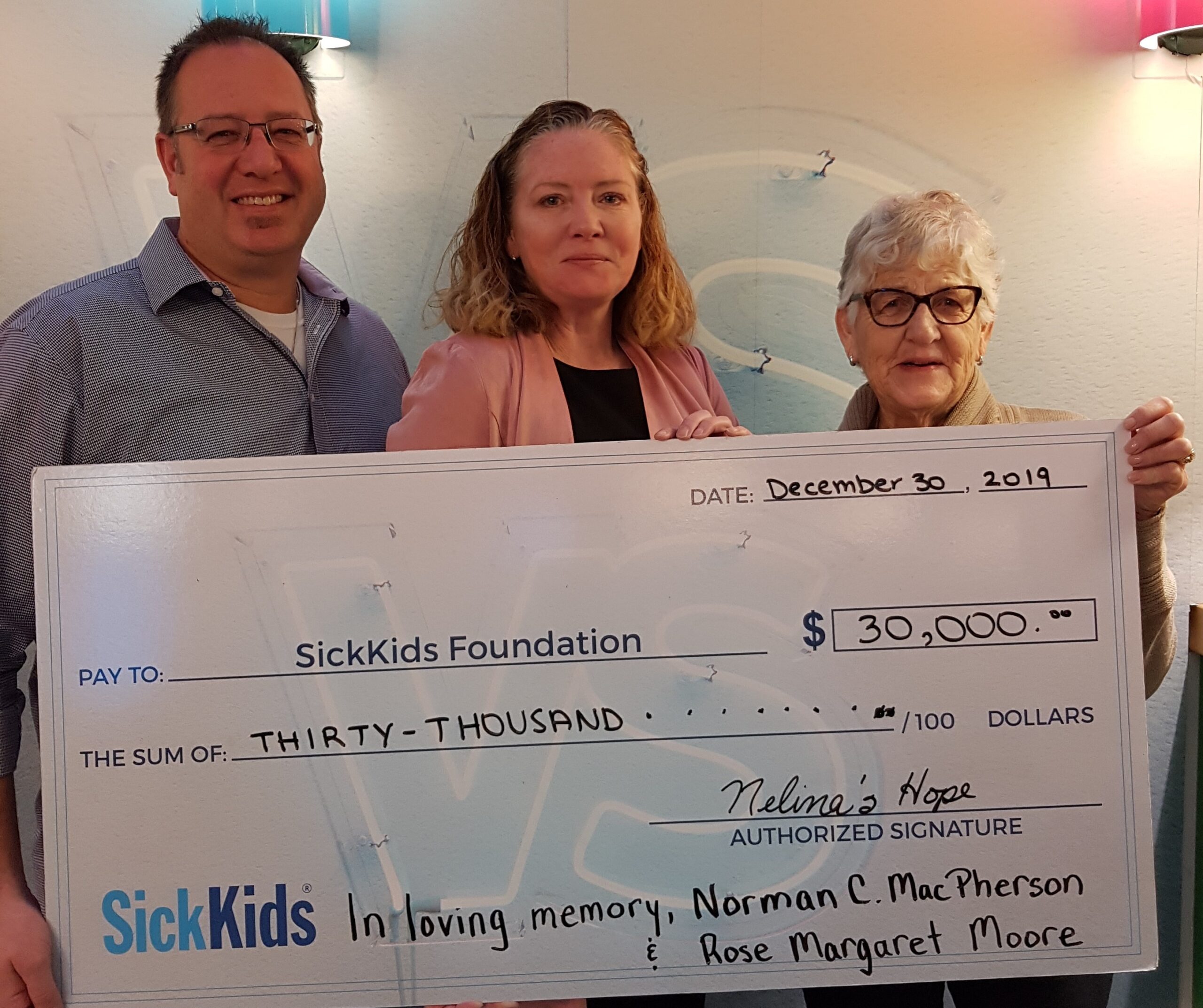
2019 & 2020 Gifts of Hope
Dr. Jim Rutka
(CED Study)
Under the coordination of Dr. Mark Souweidane, Director of Pediatric Neurological Surgery at the Weill Cornell Medicine Pediatric Brain and Spine Centre, and in partnership with Memorial Sloan-Kettering Cancer Center in New York, an exciting FDA-approved DIPG clinical trial is being conducted called convection-enhanced delivery, or CED. The patient receives a cancer-fighting drug diffused directly to the site of the tumour, bypassing the often-impenetrable blood-brain barrier and offering more effective treatment with fewer side effects. SickKids is honoured to be one of the sites chosen to participate in this trial.
(MRI Focused Study)
SickKids partnered with Sunnybrook Health Sciences Centre scientists, who made history using an early-stage specialized procedure called High-Intensity Focused Ultrasound (HIFU) to target and destroy brain tumours. Surgeons infuse an anti-cancer drug, then tiny, microscopic bubbles, into the bloodstream of a patient. The microbubbles are small and pass harmlessly through the circulatory system. Then they use state-of-the-art MRI-guided focused low-intensity ultrasound (sound waves) to target blood vessels in the area near the tumour and monitor its effectiveness and precision in real-time. Once the barrier is opened, drugs flow through and deposit into the tumour. The Brain Tumour Research Centre at SickKids developed a model demonstrating the feasibility of the blood-brain barrier disruption — a crucial first step. The team is discussing strategies to bring this into clinical practice.


2018 Gift of Hope
What makes Dr. Ramaswamy so unique and successful is his keen ability to investigate and learn from scientific data that has been overlooked to inform future discoveries. “We’ve been studying this disease for decades, but we haven’t gone back to learn from what didn’t work,” he explains. For example, there is a subgroup of medulloblastoma (medulloblastoma is a type of malignant brain cancer made up of 12 different subgroups) called WNT, which is the subgroup with the best outcomes. “There has been little interest in this group as they have a high survival rate, but recent efforts to eliminate or reduce radiation have been disappointing. There has not been much interest in the community to advance our knowledge of the biology of WNT tumours, even though there is a lot of data to study because they’re the obvious choice for testing in clinical trials,” explains Dr. Ramaswamy.
He began to study data from patients being treated in Brazil whereby despite delays in surgery, shoddy radiation, and only average surgical expertise, WNT patients treated there had a 100 percent survival rate. In Canada and across North America, the survival rate is less than 90 per cent. What were they doing that we weren’t? Why were over 10 per cent of our patients with WNT tumours relapsing? Dr. Ramaswamy uncovered the difference: it was the kinds of chemotherapies we were using. “If we’re going to reduce the radiation, we have to use the right chemotherapy drug,” says Dr. Ramaswamy. The results of these findings were published in Cell Reports.
2017 Gift of Hope
Labs at SickKids are bustling with researchers working tirelessly on new discoveries in DIPG. Dr. Cynthia Hawkins, neuropathologist and Garron Family Chair in Cancer Research at SickKids, is a shining star in the field. Dr. Hawkins has been conducting single-cell sequencing on DIPGs, learning what characteristics each tumour cell has, but also what role the normal cells around them have in the progression of DIPG. “We’re doing this because we need to build a multipronged approach. Figuring out not only how can we stop the cancer cells from dividing, but how can we keep these cells from spreading – then we can really take advantage of novel treatments like CED and move the bar on survival for these kids.” Dr. Hawkins continues to model and analyze different pathways that are responsible for DIPG, and how they respond to combinations of targeted drugs. She also works to ensure new data with the potential to help treat brain tumours is moved from the research lab into clinical testing as quickly and safely as possible. Her success has been an anchor and a jumping off point for much of the work being done in DIPG at SickKids.